US Drug Test Centers Blog
How Do Opioids Impact Your Heart? | US Drug Test Centers
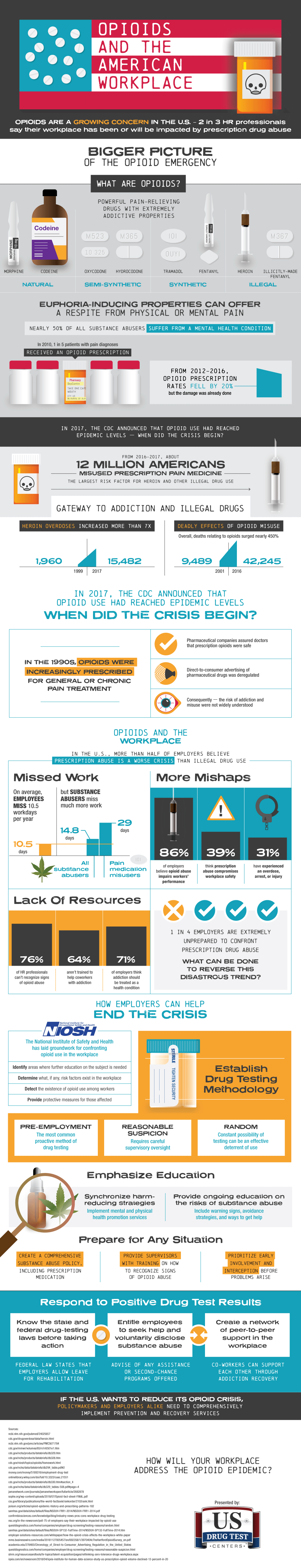
Cannabis steals a ton of headlines, but opioids are still a not-so-silent killer. In 2020, almost 75% of drug overdose deaths involved an opioid. Since 1999, overdose deaths involving opioids have increased by more than eight times. Opioids are incredibly addictive, and many people who use heroin started with prescription opioid pain relievers. What exactly do these drugs do to your body? More specifically, how do opioids impact your heart?
In this article, we’ll talk about how these drugs impact your body’s engine in both the short and long run.
What Do Opioids Do to the Body?
The way opioids work is by impacting the nerve cells in the brain and body. They block pain and help the individual feel calmer. Short-term, opioids can induce sleepiness and confusion, slow the person’s breathing, trigger nausea and vomiting, and lead to constipation. Long-term, they can lead to muscle pain, addiction, and infections of the lungs and heart.
Opioids and the Heart
Opioids change the heart’s electrical activity, largely because they affect the way that the individual breathes while they’re sleeping. This can change the heart rate and increase the chance of arrhythmia, which is when the heart doesn’t beat in its normal rhythm. For example, in atrial fibrillation, the upper chambers of the heart will beat irregularly.
People abusing opioids might experience heart palpitations — where the heart feels like it’s pounding, beating rapidly, or fluttering — shortness of breath, and weakness. All of this can increase the risk of heart failure, stroke (when blood flow to the brain is blocked), cardiac arrest (which is when the heart simply stops beating), endocarditis (inflammation of the inner lining of the heart), heart attack, hypertension (low blood pressure), and other heart-related issues.

What’s especially concerning is that cardiac arrest due to opioid abuse looks different from cardiac arrest that occurs under other circumstances. It can look as if the individual has fallen asleep. This happens because breathing and the heart rate slows down. The brain is getting less oxygen (which can lead to brain damage), and the heart eventually stops beating.
Furthermore, and perhaps ironically, opioid withdrawal can also lead to heart complications. Takotsubo cardiomyopathy (TC), also called “Broken Heart Syndrome,” happens when the left ventricle — which is the heart’s main pumping chamber — becomes weak. This can happen due to significant emotional or physical stress. TC can occur when someone is withdrawing from opioids.
Additionally, opioid withdrawal is marked by other symptoms like cravings, restlessness, anxiety, gastrointestinal issues, diaphoresis (excessive sweating), and tachycardia (an increase in heart rate).
Why are Opioids So Addictive?
Opioids tell your body to release endorphins, which are hormones that help alleviate stress or pain. Because these neurotransmitters help the brain and body feel good, when the effect wears off, the individual can find themselves wanting more. In fact, their body stops being able to produce as many endorphins on its own.
This can happen even after the short-term use of opioids. Tolerance builds, meaning that the individual needs more and more of the drug to achieve the same desired effects. Eventually, they feel like they actually need these drugs to function and survive, and that’s when it becomes an addiction.

While much opioid use starts with a prescription from a healthcare professional (more on that in a moment), an individual experiencing addiction will commonly turn to illegal drugs — like heroin — to try to get that same high.
How Did the Opioid Epidemic Even Start?
If we take a step back, we’ll see that there have been three stages of opioid addiction and overdose deaths over the last several years.
In the 1990s, healthcare providers started increasingly prescribing opioids, with OxyContin at the center of it. This eventually led to an increase in overdose deaths involving prescription opioids, which included both natural and semi-synthetic opioids and methadone. In 2010, a dramatic increase in overdose deaths involving heroin specifically began. In 2013, there was an uptick in overdose deaths involving synthetic opioids, especially fentanyl.
The COVID-19 pandemic made the situation worse. Anxiety and isolation led to an increase in drug use. Plus, there was a lack of access to healthcare. The pandemic essentially hid our country’s problem with opioids, which only compounded it.
Issues among policymakers have been a hurdle, too. Initially, Purdue Pharma — which promoted OxyContin after gaining approval from the Food and Drug Administration (FDA) — presented the drug to be less addicting than it really was. Healthcare workers (and not policymakers) alone are tasked with educating patients on the dangers of opioids and trying to mitigate risks. In some cases, opioid manufacturers are financial donors to politicians, and some government officials even leave their agencies (like the Drug Enforcement Agency, or DEA) to work in the pharmaceutical industry.
Profit is often put before the well-being of individuals, which leads to a culture where medicine is a business first, and a commitment to healthcare second.
Keep Opioid Abuse at Bay
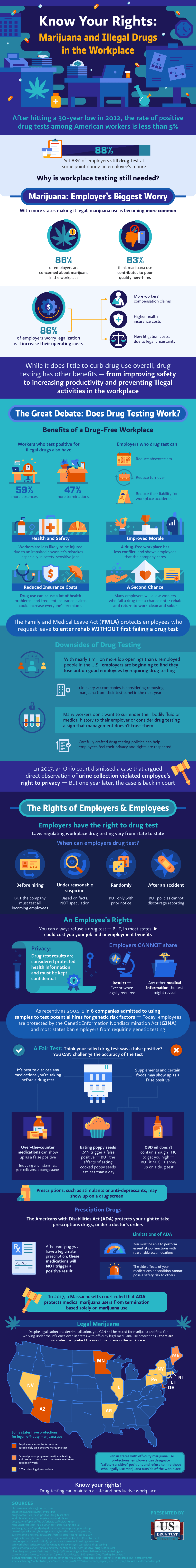
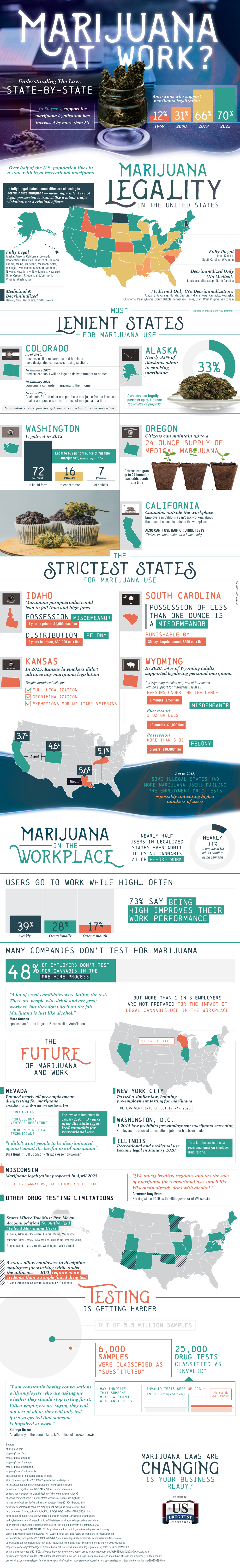
By this point, it’s probably clear how opioid abuse can not only harm the individual taking them but also the people around them. Opioids in the workplace put everyone at risk and can seriously halt operations, making employment screening an absolute must.
A drug-free workplace policy is also a must-have. This policy outlines details such as:
- What drugs the company screens for.
- Under what conditions they test individuals (pre-employment, post-accident, return-to-duty, reasonable suspicion, at random).
- What happens should an employee refuse a test.
- What happens if an employee tests positive.
US Drug Test Centers helps you keep the workplace free of drugs and alcohol. Plus, with more than 20,000 locations around the nation, getting screened is fast, easy, and convenient. Learn more about our employee testing and services.